We established the Norwich Skin Platform within the University of East Anglia, where we specialise in the development and use of physiologically relevant models of human skin.
These models are useful for research and development of potential dermatological and cosmetic products.
We have a number of academic collaborations and work with commercial partners through UEA Consultancy Ltd. We are scientists with decades of experience at the interface between the fundamental research and applied use of the skin models we have developed. Positioned as part of the Norwich Research Park, we harness the expertise of a wide range of scientists and have access to the technologies available across many different institutions.
We work with clients to develop skin models that meet their needs to identify new therapeutic targets to treat skin conditions or to evaluate their products for their potential benefits as well as to eliminate safety concerns.
Norwich Skin Platform Bacterial infection Model (NSPinfex) NEW - model in development!
However, we are happy to advise if a bespoke testing model is required.
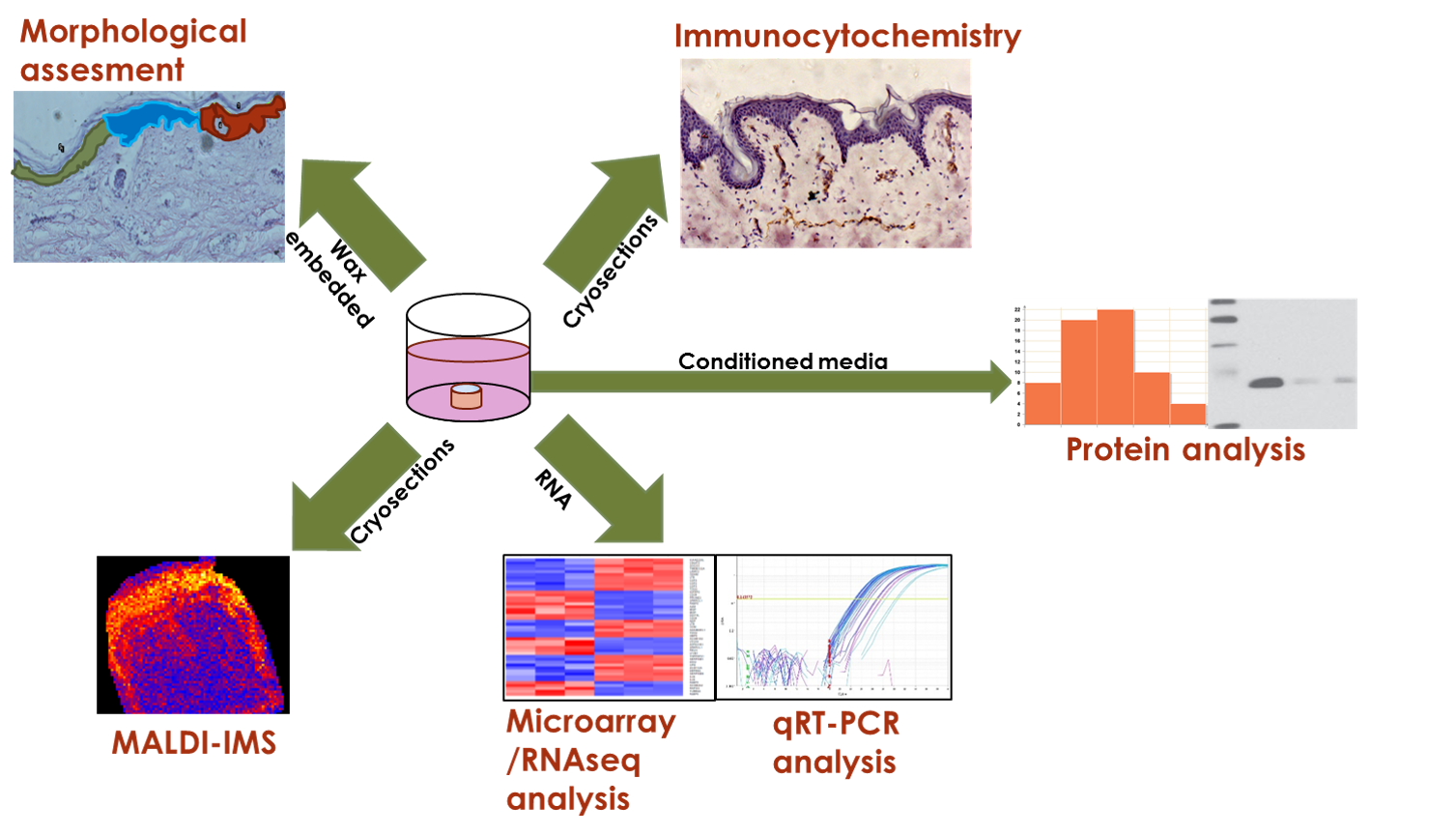
We can provide a full service of downstream analytical methods including:
Skin histology and morphometry,
Immunohistochemistry and immunolocalisation,
RNA transcript changes (RNAseq/Microarray/qRT-PCR),
Image-assisted protein mass spectrometry (MALDI-IMS),
Skin permeability and toxicity to provide data on regional and even cell-specific responses.
Contact us
e: d.bevan@uea.ac.uk
t: 01603 593816
School of Biological Sciences, Biomedical Research Centre, Norwich Research Park
Our partners



)