3D printing research at UEA could help redefine breast reconstruction surgeries for cancer patients
By: Communications

The potential to create surgical aids and biodegradable breast implants using 3D printing technology for breast reconstruction and breast-conserving surgeries is currently being researched at the University of East Anglia (UEA).
With the International Day of Women and Girls in Science coming up on 11 February, this innovation offers insight into a future where personalised, precise, and accessible solutions could help to redefine women's health.
The research project is aimed at investigating the use of 3D printing technology for medical applications, specifically how it can be used to create personalised surgical aids for breast reconstruction surgery and breast implants for breast-conserving surgery. This proof-of-concept project was funded by UEA Health and Social Care Partners (UEAHSCP), a research partnership that funds and facilitates early-stage research and innovative ideas.
The research team used a 3D scanner to capture the patient’s breast shape before the breast reconstruction surgery, to create a mould using the 3D printer. This personalised mould can be used as a surgical aid to measure the volume of the patient’s own tissue and shape for breast reconstruction, aiming to improve the quality and speed of the surgery.
The other aspect of the project involved using patient’s MRI data to create a personalised implant, which was 3D-printed using a biodegradable polymer, for breast-conserving surgery: an operation that aims to remove the cancer while keeping as much of the breast tissue and shape as possible. Once printed, the 3D scaffold implant would be placed into a patient’s breast during surgery, with the patient’s own fat injected into it, with the implant then degrading in the body slowly over time.
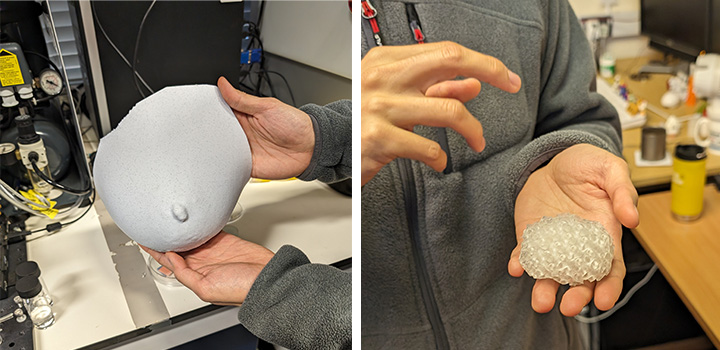 Image L-R: 3D printed breast mould; 3D printed prototype model of a biodegradable implant for breast-conserving surgery – intended to be the exact shape of a tumour.
Image L-R: 3D printed breast mould; 3D printed prototype model of a biodegradable implant for breast-conserving surgery – intended to be the exact shape of a tumour.
Ken Tam, a PhD student within UEA’s School of Pharmacy, has been working on this project under the supervision of Prof Sheng Qi, Professor of Pharmaceutical Material Science and Technology. He said:
“I firmly believe in the uniqueness of every individual and the need to address this in medical treatments. The use of 3D scanning and printing can help surgeons to do a better job. We have seen the medical applications of 3D printing in orthoepic surgery, such as making surgical guides for precise cutting. However, plastic surgery has not yet fully embraced the potential of 3D technology to improve the surgery's precision and efficiency. The personalised breast mould is one example that looks promising to be used in real practice to achieve the benefits.”
Prof Sheng Qi said: “3D printing has already been playing an important role in advancing medicine. Personalised medicine and healthcare enabled by 3D printing technology will further advance and be more widely available in the next 5-10 years. Collaborating closely with our clinicians, patients, hospitals and pharmaceutical industry, we are honoured to be a part of the exciting transformation and committed in innovating solutions to address unmet clinical needs.”
Conventional breast reconstruction often requires one or more correction surgeries after the initial operation to achieve the satisfactory shape of the breast of the patient. The personalised breast mould aims to improve the accuracy of the surgery and minimise the need for multiple surgeries, which will not only reduce the theatre time needed for each patient, but also improve the clinical outcome and patient satisfaction.
Speaking of his personal motivations, Ken said: “This project aligns perfectly with my passion for 3D printing and practical applications using scientific knowledge. Being a part of this project allows me to engage directly with cutting-edge technology and contribute to a field that has the potential to significantly improve patient outcomes. It's where my professional interests and the potential for meaningful impact converge, and that's why I decided to get involved.”
While the technology is currently under development, the potential for this project is vast. Most notably, Norfolk and Norwich University Hospital (NNUH) currently outsources its 3D printing services for some patients' cases in which personalised surgical aid, tools and surgical planning models are needed. Working in partnership with our regional Trusts, establishing a regional medical 3D printing service in Norfolk could help to significantly reduce emissions and wider environmental impacts by reducing the need to outsource the 3D printing overseas, making significant cost-savings for the regional Trusts.
The project, funded by UEAHSCP, ended on 31 August 2023 for the implant technology’s preliminary work. While the research team are currently awaiting further funding to continue this impactful research, a £3m EU project officially began on Wednesday 1 February, looking into developing a new pharmaceutical 3D printing technology for point-of-care personalised medicine manufacturing.
On Monday 5 February, the team – supported by UEAHSCP – also co-hosted their third Point-of-Care (POC) 3D printing service workshop with NNUH, which attracted more than 40 attendees from Trusts in the region. The event stimulated constructive discussions between end users, industry and regulatory experts to help formulate the UEA team’s next step forward.
Related Articles

UEA’s new high‑tech anatomy suite on schedule to open to students in September 2026
The University of East Anglia’s new high‑tech anatomy suite is on track to open to students in September 2026.
Read more
Norfolk MPs call on Government to urgently prioritise ‘underserved’ dental areas
A group of Norfolk MPs, all representing different political parties, have come together to call unanimously for the Government to prioritise the East of England in dental training.
Read more
MRI scan breakthrough could spare thousands of heart patients from risky invasive tests
Doctors may soon be able to tell just how sick a heart failure patient really is by using a routine MRI scan, thanks to new research from the University of East Anglia (UEA).
Read more